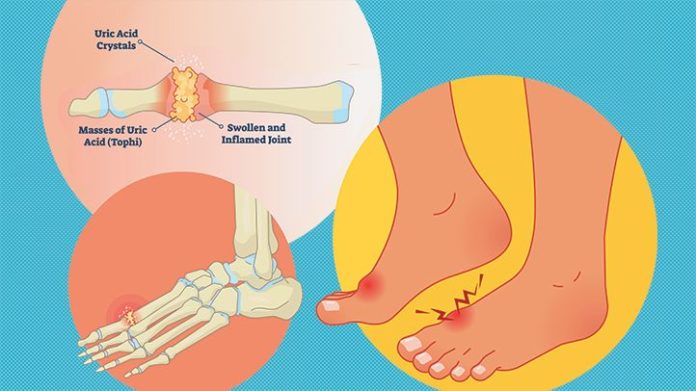
Gout is a crystalline or inflammatory form of arthritis in which high levels of serum urate cause painful, swollen, stiff joints. (1) For some people gout looks like a sudden swelling at the base of the big toe.
Intense Big Toe Pain From Gout: A Classic Symptom of an Attack
While the big toe is the most common place for a gout attack to happen, gout can also affect surrounding joints in the foot, ankle, and knee.
People with gout typically experience flare-ups, or attacks, of symptoms followed by periods with no symptoms. The attacks typically last 3 to 10 days. Some people go months or even years without a gout attack after having one. In other people, attacks may become more frequent over time.
Gout can be difficult to diagnose. Once it’s diagnosed, it can be treated with medication and lifestyle changes.
Signs and Symptoms of Gout
Pain is the most dramatic, the most common, and the most noticeable symptom of gout. For many people, the first gout attack (or flare-up) occurs in the big toe.
Other Symptoms of Acute Gout or a Gout Attack
- Sudden crushing or throbbing pain in one or a few joints (often in the big toe, knee, or ankle) that may last for a few days
- Sometimes an acute gouty arthritis attack has a sudden onset at nighttime. The big toe joint pain may be so severe that even the weight of bedsheets causes discomfort.
- Joints that appear swollen and inflamed, with reddish-purple skin that may feel warm
Chronic Gout Signs and Symptoms
- Compared with the dramatic nature of acute gout pain, chronic gout pain is more of a soreness or persistent ache.
- Pain that tends to be a more continuous feeling of dull aching or soreness in the joints
- Hard white deposits or lumps under the skin, called tophi, found on the elbows, ears, or fingers.
Learn More About Gout Signs and Symptoms
Who Gets Gout? Gout Risk Factors
Gout happens when too much uric acid builds up in the body. Uric acid is a normal waste product in the blood resulting from the breakdown of certain foods. (2) Uric acid usually passes through the kidneys and is eliminated from the body in urine. But it can build up in the blood and form painful, spiky crystals in your joints. This may happen if the body is making too much uric acid or if the kidneys are having a hard time filtering it out.
Having too much uric acid in the blood is a condition called hyperuricemia. (3) Certain foods, medicines, and lifestyle factors can cause high uric acid levels in the blood, triggering a gout attack.
Your risk of gout goes up when your diet is high in naturally occurring compounds called purines. When purines break down in the body, they cause uric acid to form. Purines are found in certain high-protein foods and some drinks. It used to be thought that gout was caused only by lifestyle and diet, but new research has found that's not true; instead, gout is thought to have a genetic link. Diet, however, does play a role in the disease.
Other risk factors for gout include:
- Being a man
- Being overweight
- Consuming excessive amounts of alcohol regularly
- A family history of gout
- High blood pressure
- Hypothyroidism
- Chronic kidney disease
- Obstructive sleep apnea
- Type 2 diabetes
- Health conditions that cause rapid turnover of cells (including some cancers, psoriasis, and hemolytic anemia)
- Kelley–Seegmiller syndrome or Lesch–Nyhan syndrome (rare disorders that affect how the body deals with uric acid)
When to Get Tested for Gout
If you’ve been experiencing gout pain and other symptoms, see your primary care doctor. Primary care physicians can often diagnose and treat gout or refer you to a rheumatologist or gout specialist for testing or treatment.
Prognosis of Gout
The first gout attacks usually affect only one joint and subside after a few days. Subsequent flare-ups may affect more joints — either at the same time or one after the other. If untreated, these later attacks can last up to three weeks. Attacks then snowball in frequency, occurring several times annually.
As the disease progresses, gout becomes more aggressive in patients who develop symptoms before the age of 30, and whose baseline serum uric acid level is greater than 9.0 milligrams per deciliter (mg/dL). If caught and treated early, people with gout can live a relatively normal life. Some patients do not respond to treatment because they fail to follow protocols, have alcoholism, or are undertreated by physicians. (4)
Treatment for Gout and Gout Attacks
As soon as you’ve been diagnosed with gout, your doctor will aim to reduce your pain ASAP. In May 2020, the American College of Rheumatology (ACR) updated its guidelines for gout treatment for the first time in eight years. There is more evidence in support of early diagnosis and treatment (especially for people with comorbidities such as kidney disease); treat-to-target (T2T) protocols; and allopurinol as a first-line agent.
Medication Options
A number of different drugs can be used to treat gout flare-ups.
- Nonsteroidal anti-inflammatory drugs (NSAIDS) These medications block the prostaglandins, which promote pain and inflammation. Common over-the-counter ones include ibuprofen, aspirin, and naproxen; common prescription ones are celecoxib, ketoprofen and naproxen sodium. You must talk to your doctor before you take these.
- Colchicine If you are unable to tolerate NSAIDS, your doctor may prescribe colchicine, but it must be taken daily. There can be side effects such as diarrhea, nausea, vomiting, and abdominal cramps.
- Corticosteroids Taken orally or injected directly into affected joint, the most common corticosteroids used for gout are prednisone, prednisolone, and methylprednisolone.
- Uric-acid-lowering medicine, such as losartan or allopurinol. These drugs must be taken daily and used long-term. The new gout guidelines recommend taking these with a three- to six-month course of NSAIDS.
Alternative and Complementary Therapies
Many complementary and alternative medicine (CAM) approaches for managing gout focus on diet, weight loss, and exercise.
Your risk of gout goes up when your diet is high in naturally occurring compounds called purines. When purines break down in the body, they cause uric acid to form. In most cases, people who have gout will still need medication even when they follow a diet for gout. That said, tweaking your diet can be a powerful way to help manage gout and gout symptoms. Some research suggests that food changes alone can lower your uric acid levels by up to 15 percent, according to the Institute for Quality and Efficiency in Health Care.
The main principles of a gout diet are basically the same as those of any healthy diet: Reduce calorie consumption if you are overweight; opt for unrefined carbohydrates like fruits, vegetables, and whole grains; limit your intake of sugar, organ meats (such as kidney, liver, or sweetbreads), and saturated fats.
Avoid Foods That May Trigger Gout
Purines are found in certain high-protein foods, such as certain types of seafood (including mackerel, herring, scallops, anchovies, and sardines), and red meat and organ meat (especially beef kidneys, liver, game meats, and sweetbreads). Avoid drinks that may trigger gout:
- Alcoholic beverages (beer, whiskey, gin, vodka, and rum)
- Sugary drinks (sodas, juices, energy drinks)
- Coffee and other caffeinated beverages. While some studies show that caffeine can actually protect against gout pain, others find that sudden spikes in caffeine intake can trigger an attack.
RELATED: Gout Diet and Eating to Help Prevent Gout
Can You Drop 8 Pounds? Weight Loss Helps Prevent Gout
If you’re overweight, you are likely to have higher-than-normal uric acid levels, a primary risk factor for developing gout. That’s why weight loss is an important part of a gout diet.
Losing weight may help lower uric acid levels and reduce the risk that you will experience future gout attacks. In fact, a weight loss of about eight pounds or more led to long-term reductions in uric acid levels and gout attacks in overweight or obese people, according to a review of studies published in 2017 in the Annals of the Rheumatic Diseases.
While some people with gout benefit from cutting back on foods that are high in purine, a chemical that contributes to uric acid formation, it is not clear how much purine intake makes a difference. You don’t have to avoid all high-purine foods. Moderate changes to your eating style may help you feel better and reduce gout risks, and research suggests that purine-rich vegetables don’t trigger gout. High-purine foods such as lentils and beans can be a smart source of lean protein.
Get Appropriate Exercise
Many people with gout avoid exercise because they fear it will make the inflamed joint worse. There are special programs that help people with all kinds of arthritis adapt their exercise needs. The CDC has a list of recommended programs that you can find in your local hospital, community center, or YMCA.
Learn More About Gout Treatment
Prevention of Gout
In addition to diet, exercise, and weight loss, avoid these medications that can trigger gout, if you can:
- Diuretics (used to treat high blood pressure or heart disease)
- Salicylate-containing drugs (such as aspirin)
- Niacin (vitamin B3 and nicotinic acid)
- Cyclosporine (an immune-suppressing drug)
- Levodopa (used to treat Parkinson’s disease)
Research and Statistics: How Prevalent Is Gout in the United States?
Research published in the journal Arthritis & Rheumatology found that gout rates in the United States have been climbing steadily over the past 50 years, likely because of increases in obesity and high blood pressure. (8)
Gout is the most common type of inflammatory arthritis among men. It’s more common in men than women. About 6 percent of men in the United States have gout, while only about 2 percent of women have it. Women rarely develop gout before reaching menopause. (1)
Gout is rare in children and young adults.
Resources We Love
There are many online resources for information and support for people with gout. Check out our Gout Resource Center.
Editorial Sources and Fact-Checking
- Gout. National Institute of Arthritis and Musculoskeletal and Skin Diseases. April 30, 2016.
- Gout. Centers for Disease Control and Prevention. July 27, 2020.
- Gout. Arthritis Foundation.
- Edwards NL. Gout. Merck Manual Professional Version. April 2018.
- Symptoms and Diagnosis of Gout: Arthritis/Acute Gout Attack. Johns Hopkins Arthritis Center.
- Interventions for Tophi in Gout. Cochrane Database of Systematic Reviews Journal of Rheumatology Supplement. September 2014.
- Gout. MedlinePlus. April 24, 2017.
- Zhu Y, Pandya B, Choi H. Prevalence of Gout and Hyperuricemia in the U.S. General Population: The National Health and Nutrition Examination Survey 2007–2008. Arthritis & Rheumatology. September 2011.
- Pseudogout. Mayo Clinic. July 2, 2015.