Meningitis occurs when there is an inflammation of the membranes that cover and protect the brain and spinal cord (the meninges), according to the Centers for Disease Control and Prevention (CDC). (1)
Viral infections are the most common cause of meningitis in the United States, but the illness can also be caused by bacterial, parasitic, and fungal infections, according to the Mayo Clinic. (2) Other types of infections can also cause meningitis, and there are noninfectious causes as well, such as injuries, cancer, and certain medication. (1)
Viral meningitis, the most common type of meningitis, is typically mild and frequently goes away on its own. (2) However, bacterial meningitis can be life-threatening within days if it’s not treated or lead to permanent brain damage, so be sure to seek medical care immediately if you think you may have the infection.
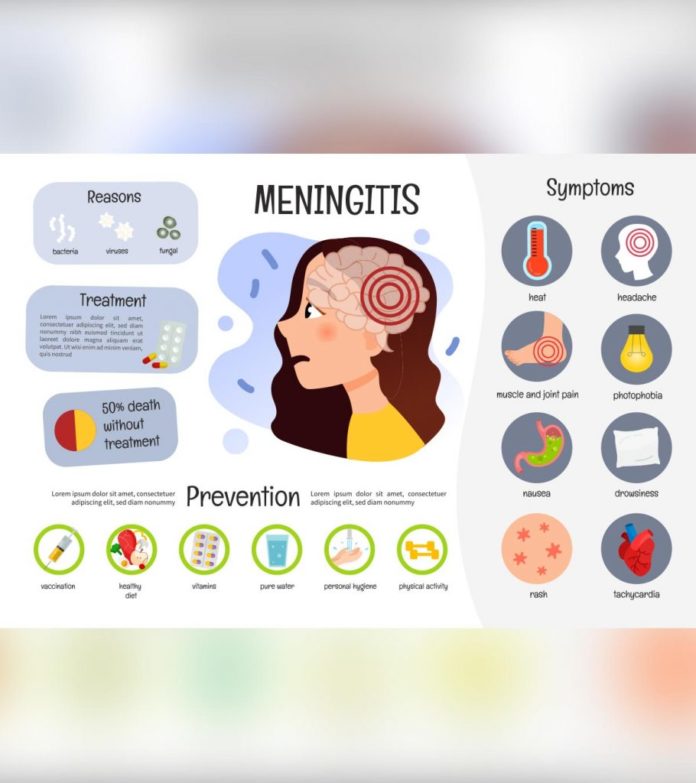
Signs and Symptoms of Meningitis
Early meningitis symptoms may seem like flu symptoms and may present over several hours or several days, per the Mayo Clinic. (2)
Signs and symptoms in people over the age of 2 may include:
- High fever that comes on suddenly
- Stiff neck
- Severe headache that seems unusual
- Headache with nausea or vomiting
- Confusion or trouble concentrating
- Seizures
- Sleepiness or difficulty waking up
- Sensitivity to light
- Lack of appetite or thirst
- Skin rash (in some types of meningitis — e.g., meningococcal meningitis)
Signs and symptoms in newborns and infants may include:
- High fever
- Nonstop crying
- Atypical sleepiness or irritability
- Lack of activity or sluggishness
- Failure to feed well
- A bulge in the soft spot on top of a baby's head (fontanel)
- Stiffness in a baby's body and neck
- A baby that is difficult to comfort
Learn More About Signs and Symptoms of Meningitis
How Is Meningitis Diagnosed?
Doctors diagnose meningitis by taking a medical history, conducting a physical exam, and administering diagnostic tests, per the Mayo Clinic. (9) Your healthcare provider may look for signs of infection around the head, ears, throat, and the skin along the spine.
Tests used to diagnose meningitis include:
- Blood Cultures Blood cultures may be ordered to detect bacteria.
- Computerized tomography (CT) or Magnetic resonance imaging (MRI) scans of the head may reveal swelling or inflammation, and X-rays or CT scans of the chest or sinuses may also show infection.
- Spinal Tap A spinal tap (lumbar puncture) is done to collect cerebrospinal fluid (CSF) and definitively diagnose meningitis. If you have meningitis, the CSF frequently shows a low sugar (glucose) level as well as an elevated white blood cell count and increased protein.
- CSF Analysis CSF analysis may be done to pinpoint which bacteria caused the meningitis. In cases of viral meningitis, your doctor may order a DNA-based test known as a polymerase chain reaction (PCR) amplification or a test to check for antibodies against certain viruses.
Prognosis of Meningitis
Some cases of meningitis get better without treatment in a few weeks, according to the Mayo Clinic. In other cases, emergency treatment is necessary to prevent serious complications, including death. (2)
Viral meningitis is typically mild and frequently goes away on its own.
Early diagnosis and treatment of bacterial meningitis are critical to prevent permanent neurological damage, according to MedlinePlus. (10)
In most cases, people with very mild meningitis can make a full recovery, per the National Institute of Neurological Disorders and Stroke. (11)
Treatment and Medication Options for Meningitis
Treatment for Bacterial Meningitis
Acute bacterial meningitis is a medical emergency that must be treated right away, even before results of the CSF analysis are known, according to the Mayo Clinic. (9)
Medication Options
Medication for bacterial meningitis may include:
- Intravenous antibiotics
- Corticosteroids to reduce inflammation
Your doctor may also drain any infected sinuses or mastoids, which are the bones behind the outer ear that connect to the middle ear.
Treatment for Viral Meningitis
Antibiotics can't cure viral meningitis. For mild cases, treatment usually includes bed rest and lots of fluids.
Medication Options
Medication options for viral meningitis include:
- Over-the-counter pain medication (for fever and body aches)
- Corticosteroids to reduce swelling in the brain
- Anticonvulsant medication to control seizures
- Antiviral medication, if a herpes virus caused your meningitis
Treatment for Other Types of Meningitis
There are various treatments for other types of meningitis, including
- Antifungal medication to treat fungal meningitis
- Corticosteroids to treat noninfectious meningitis
Learn More About Treatment for Meningitis: Medication, Alternative and Complementary Therapies, Surgery Options, and More
Prevention of Meningitis
The following steps can help prevent meningitis, per the Mayo Clinic: (2)
- Wash your hands well and teach children to do the same.
- Don't share drinks, foods, straws, eating utensils, lip balms, or toothbrushes with other people.
- Stay healthy and boost your immune system by getting enough rest, exercising regularly, and eating a healthy diet with plenty of fresh fruit, vegetables, and whole grains.
- When you need to cough or sneeze, cover your mouth and nose.
- If you're pregnant, reduce your risk of listeriosis by cooking meat, including hot dogs and deli meat, to 165 degrees F. Avoid cheeses made from unpasteurized milk, and eat only cheeses made with pasteurized milk.
Vaccines for Meningitis
According to the Mayo Clinic, you can prevent bacterial meningitis by keeping yourself and your children up-to-date on the following vaccines:
- Haemophilus Influenzae Type B (Hib) Vaccine Children in the United States routinely receive this vaccine starting at about 2 months old. It’s also recommended for some adults, including people who have sickle cell disease or AIDS and individuals who don't have a spleen.
- Pneumococcal Conjugate Vaccine (PCV13) This vaccine is routinely given to American children younger than 2 years old. Additional doses are recommended for children older than 2 years old and younger than 5 years old who are at increased risk of pneumococcal disease, such as those who have chronic heart or lung disease or cancer.
- Pneumococcal Polysaccharide Vaccine (PPSV23) This vaccine may be recommended for older children and adults who need protection from pneumococcal bacteria, including all adults older than 65; younger adults and children age 2 and older who have weak immune systems or illnesses such as heart disease, diabetes, or sickle cell anemia; and anyone who doesn't have a spleen.
- Meningococcal Conjugate Vaccine The CDC recommends that children receive a single dose of this vaccine at age 11 or 12, and a booster shot at age 16. It can also be given to children between 2 months old and 10 years old who are at increased risk of bacterial meningitis, and to unvaccinated people who have been exposed in outbreaks.
Research and Statistics: How Many People Have Meningitis
At least 1.2 million cases of bacterial meningitis are estimated to occur worldwide each year, according to the World Health Organization. (12)
While enteroviruses cause most cases of viral meningitis and most people are exposed to these viruses, fewer than 1 in every 1,000 people infected with enteroviruses actually develops meningitis. (13)
Related Conditions and Causes of Meningitis
Encephalitis
Encephalitis is inflammation of the brain, as opposed to meningitis, which is inflammation of the membranes that surround the brain and spinal cord. (10) The illness is usually caused by a viral infection. In most cases, people with very mild encephalitis can make a full recovery.
Septicemia
The same bacteria that cause bacterial meningitis can also be associated with sepsis, or septicemia, which is the medical term for a bacterial infection that spreads throughout the body. (4) Septicemia is the body's extreme response to an infection, and it can be fatal without prompt treatment, according to Johns Hopkins Medicine. (15)
RELATED: What Is Sepsis? Symptoms, Causes, Diagnosis, Treatment, and Prevention
Resources We Love
Centers for Disease Control and Prevention
The CDC is the nation's health protection agency. Its website offers information about the types of meningitis, plus information about how it spreads.
Mayo Clinic
Mayo Clinic is a nonprofit organization that specializes in clinical practice, education, and research. Its website offers information about the symptoms, causes, risk factors, complications, and prevention of meningitis, plus diagnosis and treatment.
MedlinePlus
MedlinePlus is a service of the National Library of Medicine (NLM), the world's largest medical library, which is part of the National Institutes of Health (NIH). It offers information about the causes, symptoms, diagnosis, treatment, prognosis, complications, and prevention of meningitis.
Learn more about additional resources and support for meningitis
Editorial Sources and Fact-Checking
- Meningitis. Centers for Disease Control and Prevention. January 21, 2020.
- Meningitis. Mayo Clinic. October 1, 2020.
- Viral Meningitis. Centers for Disease Control and Prevention. August 6, 2019.
- Bacterial Meningitis. Centers for Disease Control and Prevention. August 6, 2019.
- Fungal Meningitis. Centers for Disease Control and Prevention. August 6, 2019.
- Parasitic Meningitis. Centers for Disease Control and Prevention. August 6, 2019.
- Amebic Meningitis. Centers for Disease Control and Prevention. August 6, 2019.
- Non-Infectious Meningitis. Centers for Disease Control and Prevention. August 6, 2019.
- Meningitis. Mayo Clinic. October 1, 2020.
- Meningitis. MedlinePlus. September 16, 2020.
- Meningitis and Encephalitis Fact Sheet. National Institute of Neurological Disorders and Stroke. March 16, 2020.
- Control of Epidemic Meningococcal Disease. WHO Practical Guidelines. 2nd edition. World Health Organization.
- Viral Meningitis. Wisconsin Division of Public Health.
- Meningococcal Disease in Other Countries. Centers for Disease Control and Prevention. May 31, 2019.
- Septicemia. Johns Hopkins Medicine.