Whooping cough (pertussis) is a very contagious respiratory disease caused by the bacteria Bordetella pertussis. When this bacteria infects the linings of the lungs, it causes significant inflammation and swollen airways. The result is intense, uncontrollable coughing.
Causes and Risk Factors of Whooping Cough
Here’s what you need to know about who’s at risk:
- Infants Under 2 Months Old The youngest babies are also the most vulnerable to whooping cough and its complications. Not only are their immune systems still developing, but young babies cannot start receiving their whooping cough vaccinations until they’re 2 months old. Until then, they only have their mother’s antibodies to project them. (This, of course, is only if mom got her whooping cough vaccine during pregnancy.)
- Babies Under 6 Months Old These children are at high risk for complications from whooping cough, including pneumonia, notes the CDC.
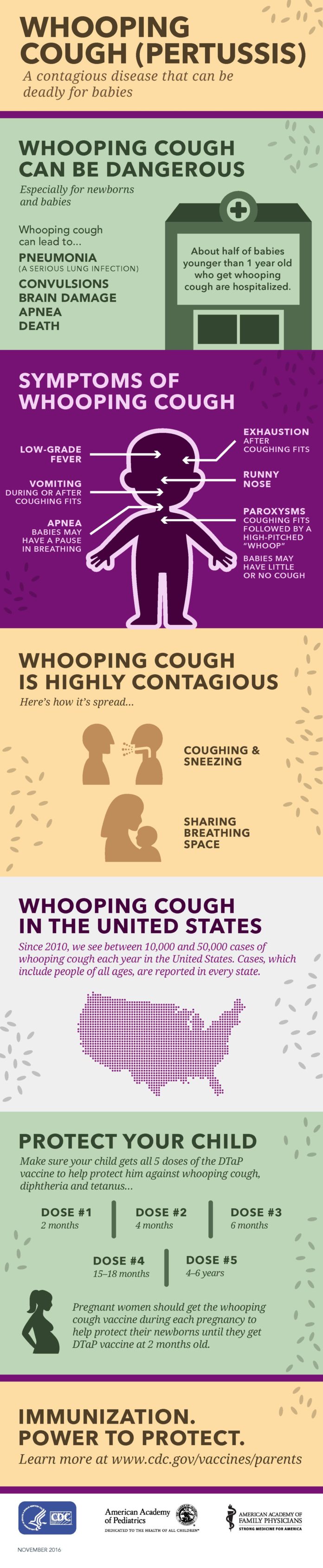
- Babies Under 12 Months Old According to the CDC, about half of babies younger than 1 year old who contract whooping cough end up hospitalized.
- Kids Under 6 Years Old Children don’t receive their final whooping cough vaccine booster shot until somewhere between the ages of 4 and 6, says the CDC.
- Teenagers and Adults The whooping cough vaccine administered in childhood eventually wears off, leaving teenagers and adults susceptible during an outbreak.
Duration of Whooping Cough
Treatment and Medication Options for Whooping Cough
If an infant has a severe case of the illness, hospitalization may be required. In the hospital, an IV may be administered to replace lost fluids, and the throat may need to be suctioned to clear away excess mucus.
Alternative and Complementary Therapies
- Using a cool-mist vaporizer to help loosen mucus and soothe irritated lungs and cough
- Eating small, frequent meals to help prevent vomiting
- Drinking plenty of water to avoid dehydration
- Keeping your home free from irritants like smoke, dust, or chemical fumes that irritate the lungs
Prevention of Whooping Cough
Getting vaccinated is the number one way to prevent whooping cough. According to the CDC, children who haven’t received their DTaP vaccines are at least 8 times more likely to get sick than those who’ve received all five doses of that vaccine. (DTaP vaccines prevent against diphtheria, tetanus, and pertussis.)
Right now, there are two available vaccines that do the job in the United States: DTaP for children under 7 years old and Tdap for adolescents and adults. (Tdap is the name for the one-shot vaccine against tetanus, diphtheria and pertussis that’s given to people 11 years and older.)
Here’s who should get shots and when:
- Infants and Young Children Babies should receive their first whooping cough vaccination at 2 months old, followed by a second and third dose at 4 months and 6 months. The fourth vaccination should be administered between 15 and 18 months, followed by the fifth and final shot between 4 and 6 years old, according to the U.S. Department of Health and Human Services.At least 90 percent of kids are fully protected after getting all five doses of DTaP, per the CDC.
- Preteens and Teens DTaP’s ability to prevent whooping cough slowly decreases over time. For instance, if a child received her last DTaP at age 6, by the age of 11, that child’s chance of being fully protected hovers at 70 percent. As such, the CDC recommends that all children between the ages of 11 and 12 get a booster shot of the Tdap vaccine.
- Adults 19 and Older Didn’t get the Tdap booster as a teen? You’ll want to make sure you get it now. In addition, a single Tdap dose should be given to adults who are in contact with infants as well as healthcare workers, according to the CDC.
- Pregnant Women The CDC recommends that all pregnant women get a Tdap shot between the 27th and 36th week of each pregnancy. This way, you create protective antibodies to pass onto the baby before birth, helping to provide short-term protection against whooping cough and the related complications, notes the CDC.Doing so lowers the risk of contracting whooping cough by about 91 percent during the first two months of baby's life, according to the 2017 report in the journal Pediatrics.
No vaccine is 100 percent effective, but it is the very best protection available. Plus, if an individual does contract whooping cough after getting the vaccines, they are less likely to experience a serious infection.
- Are immunocompromised
- Have moderate to severe asthma
- Work in neonatal intensive care units, childcare settings, maternity wards
- Are infants younger than a year, particularly those who are younger than 4 months
- Women in the third trimester of pregnancy
Complications of Whooping Cough
- Pneumonia (babies and children)
- Seizures (babies and children)
- Encephalopathy (inflammation of the brain)
- Hernia
- Collapsed lung
Related Conditions of Whooping Cough
Resources We Love
Centers for Disease Control and Prevention (CDC)
Here you’ll find all the vetted and trusted info on whooping cough that you could possibly need. The CDC is also a great place to learn about all childhood vaccinations, with helpful videos and schedules that can help you stay on schedule for these potentially life-saving shots.
American Academy of Pediatrics (AAP)
There are 67,000 pediatricians who are members of the AAP, a leading national voice on children’s health. The parent-forward version of their website, called HealthyChildren.org, is a superb resource on all early childhood conditions, including chronic cough, whooping cough, and similar infections. There’s also the Symptom Checker, where parents can plug in various symptoms (like cough) to get specific tips about how to help and when to call the doctor.
Editorial Sources and Fact-Checking
References
- 2019 Provisional Pertussis Surveillance Report. Centers for Disease Control and Prevention. February 2020.
- Whooping Cough (Pertussis). Kids Health. February 2016.
- Pertussis (Whooping Cough): Signs and Symptoms. Centers for Disease Control and Prevention. August 7, 2017.
- Pertussis. Merck Manuals: Consumer Version.
- Five Things to Know About Whooping Cough. American Lung Association. January 10, 2019.
- Pregnancy and Whooping Cough: Deadly Disease for Babies. Centers for Disease Control and Prevention. June 29, 2017.
- Pregnancy and Whooping Cough: Vaccinate Your Baby. Centers for Disease Control and Prevention. June 29, 2017.
- Pertussis (Whooping Cough) Best Practices for Healthcare Professionals on the Use of Polymerase Chain Reaction (PCR) for Diagnosing Pertussis. Centers for Disease Control and Prevention. August 7, 2017.
- Whooping Cough: Diagnosis and Treatment. Mayo Clinic. October 9, 2019.
- Pertussis (Whooping Cough): Treatment. Centers for Disease Control and Prevention. October 25, 2019.
- Pertussis (Whooping Cough): Diagnosis and Treatment. Centers for Disease Control and Prevention. August 7, 2017.
- Whooping Cough (Pertussis). U.S. Department of Health and Human Services. January 2020.
- Pregnancy and Whooping Cough: Get the Whooping Cough Vaccine During Each Pregnancy. Centers for Disease Control and Prevention. August 25, 2020.
- Baxter R, Bartlett J, Fireman B, Lewis E et al. Effectiveness of Vaccination During Pregnancy to Prevent Infant Pertussis. Pediatrics. May 2017.
- Pertussis (Whooping Cough): Postexposure Antimicrobial Prophylaxis. Centers for Disease Control and Prevention. November 18, 2019.
- Razzaghi H, Kahn KE, Black CL, et al. Influenza and Tdap Vaccination Coverage Among Pregnant Women — United States, April 2020. CDC: Morbidity and Mortality Weekly Report. October 2, 2020.
- Disparities Details by Race and Ethnicity for 2018. Office of Disease Prevention and Health Promotion.
- Zerbo O, Bartlett J, Goddard K, et al. Acellular Pertussis Vaccine Effectiveness Over Time. Pediatrics. July 2019.
- Pertussis. National Organization for Rare Disorders.
- Pertussis (Whooping Cough): Frequently Asked Questions. Centers for Disease Control and Prevention. November 18, 2019.
- Pertussis: Fast Facts. Centers for Disease Control and Prevention. August 7, 2017.
- Pertussis: Summary of Vaccine Recommendations. Centers for Disease Control and Prevention. January 22, 2020.
- Maurer J, Harris K, Uscher-Pines L. Can Routine Offering of Influenza Vaccination in Office-Based Settings Reduce Racial and Ethnic Disparities in Adult Influenza Vaccination? Journal of General Internal Medicine. December 2014.
- Hamel L, Lopes L, Muñana C, et al. KFF — The Undefeated Survey on Race and Health. Kaiser Family Foundation. October 13, 2020.
Sources
- Pertussis (Whooping Cough): Causes and Transmission. Centers for Disease Control and Prevention. August 7, 2017.
- Whooping Cough. HealthyChildren.org. November 21, 2015.
- Whooping Cough: Symptoms and Causes. Mayo Clinic. October 9, 2019.