Deep vein thrombosis (DVT) is caused by a blood clot that forms in one or more of the deep veins in your body, typically in your legs. Clots can also occur in the arms.
Fortunately, DVT is preventable and treatable if detected early.
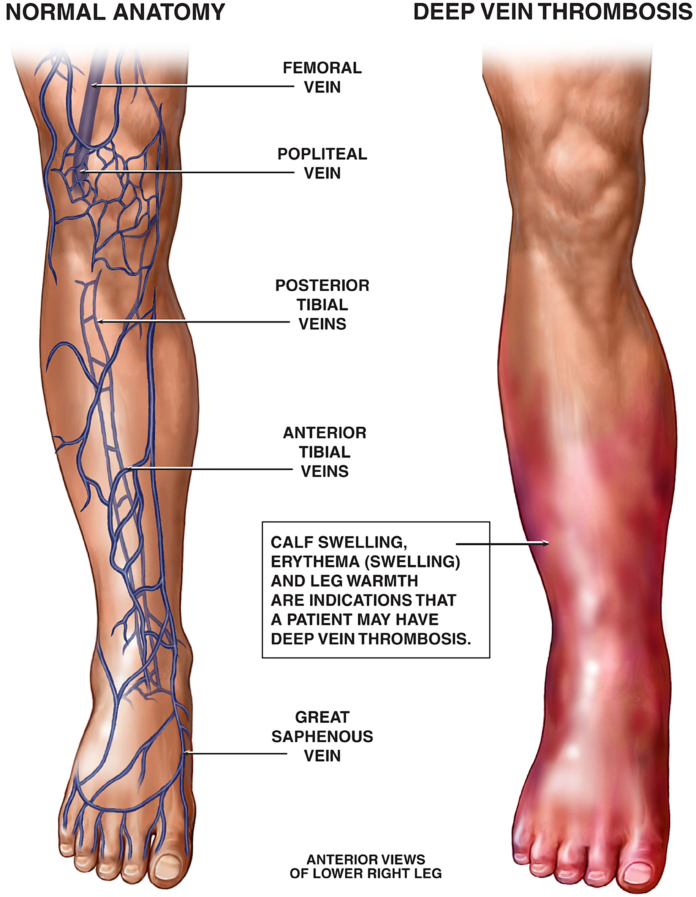
Signs and Symptoms of DVT
If you have DVT, you may experience discomfort in your leg. However, the condition can occur without any symptoms.
- Swelling in one leg (it’s rare that swelling would occur in both legs)
- Pain in the affected leg
- Skin that is red or discolored on the affected leg
- Skin that is warm to the touch on the affected leg
If you see signs or symptoms of DVT, talk to your doctor. If you have symptoms of a pulmonary embolism, seek emergency medical assistance immediately.
- Unexplained or sudden shortness of breath
- Chest pain or discomfort that worsens when you take a deep breath or cough
- Dizziness or fainting
- Rapid pulse
- Coughing up blood
How Is DVT Diagnosed?
- Duplex Venous Ultrasound This test shows the blood flow in your deep veins so your doctor can check for clots.
- D-Dimer Blood Test This checks for elevated levels of the protein D-dimer (a sign of DVT).
- Venography This X-ray of the veins in your legs and feet is another way to check for clots. It is rather invasive, so other tests are typically done first, so it is not often performed.
- CT Scan or MRI These are often done to check for blood clots in the abdomen.
Treatment and Medication Options for DVT
Anticoagulants
Anticoagulants, or blood thinners, are usually the first-choice treatment for DVT. Although anticoagulants don't break up existing clots, they can prevent the clot from growing in size and prevent new clots from forming.
When you start anticoagulation therapy by injection, your doctor will often administer the first few doses, after which you may be able to administer the injections on your own.
Injectable blood thinners include these examples:
- Lovenox (enoxaparin)
- Fragmin (dalteparin)
- Aritxtra (fondaparinux)
- Heparin
If your doctor prescribes oral anticoagulation therapy — such as Coumadin (warfarin), Xarelto (rivaroxaban), Eliquis (apixaban), or Savaysa (exoxaban) — you will typically take these medications for three months or longer.
Your doctor may recommend regular blood tests to check how long it takes for your blood to clot. All blood thinners must be taken as prescribed to avoid serious side effects.
Thrombolytics
Also known as tissue plasminogen activators, thrombolytics are given intravenously (by IV) or through a catheter positioned near an existing blood clot. They are designed to break up clots.
Thrombolytics can cause serious bleeding. They are used only in life-threatening situations and only if you are hospitalized.
Filters
If you are unable to take blood thinners for any reason, your doctor may recommend a minor surgical procedure in which a filter is inserted into a large vein in your abdomen, known as the inferior vena cava.
This filter is designed to prevent any clots that break loose from traveling to your lungs.
Surgery and Socks
In rare cases, clots may need to be removed by surgery.
Finally, wearing compression stockings on your legs can help prevent swelling associated with DVT. The pressure they create lowers the risk of blood pooling and clotting.
Complications of DVT
A pulmonary embolism occurs when a blood vessel in your lung is blocked by a blood clot that has moved from another part of your body, usually a deep vein in your leg. It can be fatal if left untreated.
Post-thrombotic syndrome (PTS) is another common complication associated with DVT. It's caused by damage to your veins from a blood clot that reduces blood flow in the affected areas. According to the CDC, one-third to one-half of people with DVT will develop PTS.
Signs and symptoms of PTS include:
- Swelling or pain in your legs
- Skin discoloration
- Skin sores
Related Conditions and Causes of DVT
DVT and COVID-19
Much attention has been paid to the risk of blood clots and the COVID-19 vaccine, but research suggests that the risk is much higher from the virus itself.
The results showed that for every 10 million people vaccinated with the AstraZeneca shot, 66 experienced a blood clot in their veins. This is compared with 12,614 per 10 million people with COVID-19.
The study also found that 143 people out of 10 million had an ischemic stroke in the 28 days after the first dose of the Pfizer vaccine, compared with 1,699 with COVID-19.
The research adds to the evidence that getting infected with COVID-19 is more serious than the potential side effect from the vaccine that protects against getting COVID-19.
Editorial Sources and Fact-Checking
- What Is Venous Thromboembolism? Centers for Disease Control and Prevention. February 7, 2020.
- Deep Vein Thrombosis (DVT). Cleveland Clinic. July 18, 2019.
- Deep Vein Thrombosis (DVT): Symptoms and Causes. Mayo Clinic. December 22, 2020.
- Deep Vein Thrombosis. American Academy of Family Physicians. September 10, 2020.
- Treating and Managing Pulmonary Embolism. American Lung Association. October 23, 2020.
- Diagnosis and Treatment of Venous Thromboembolism. Centers for Disease Control and Prevention. February 7, 2020.
- Prevent Blood Clots. Centers for Disease Control and Prevention. October 13, 2020.
- Data and Statistics on Venous Thromboembolism. Centers for Disease Control and Prevention. February 7, 2020.
- Risk Factors for Venous Thromboembolism (VTE). American Heart Association. March 30, 2017.
- Pregnant? Don’t Overlook Blood Clots. Centers for Disease Control and Prevention. February 7, 2020.
- Hippisley-Cox J, Patone M, Mei X, et al. Risk of Thrombocytopenia and Thromboembolism After COVID-19 Vaccination and SARS-CoV-2 Positive Testing: Self-Controlled Case Series Study. The BMJ. August 27, 2021.