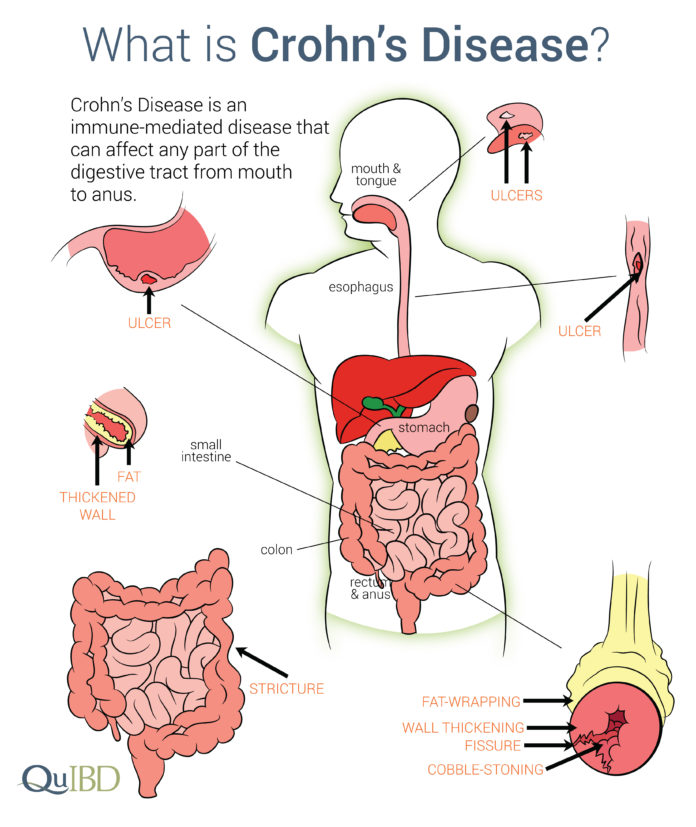
Crohn's disease is a chronic digestive disorder that causes inflammation and damage in the digestive tract.
The disease belongs to a group of conditions called inflammatory bowel diseases (IBD).
There's no cure for Crohn's disease, but there are many treatments to help manage its symptoms.
Types of Crohn’s Disease
There are several different types of Crohn’s disease, categorized by the area of the digestive tract affected.
Ileitis This form of Crohn’s disease affects only the ileum.
Crohn’s Colitis Also known as granulomatous colitis, this form of the disease affects only the colon.
Gastroduodenal Crohn’s Disease This form of the disease affects both the stomach and the beginning of the small intestine (duodenum).
Signs and Symptoms of Crohn’s Disease
No two people experience Crohn’s disease in exactly the same way.
Your symptoms will depend on what areas of your bowel are affected, as well as how advanced your disease is and how well your treatments are working.
Most people with Crohn’s disease experience inflammation in both their small intestine and their large intestine (colon), which often causes diarrhea and abdominal pain or cramping.
Other common digestive symptoms include rectal bleeding, nausea or loss of appetite, an urgent need to defecate, and constipation.
Crohn’s disease can also cause weight loss, fatigue, and symptoms outside the digestive system, like joint pain, red or itchy eyes, and inflamed or bumpy skin.
Learn More About Crohn's Disease Symptoms
Causes and Risk Factors of Crohn’s Disease
The exact causes of Crohn's disease are unknown.
Experts believe a combination of genetic and environmental factors contribute to a person's risk for the disease.
Some risk factors for Crohn's disease include:
How Is Crohn’s Disease Diagnosed?
The first step to diagnosing Crohn’s disease is complete medical history, a physical exam, and a series of tests to rule out other conditions that may cause similar symptoms. These include irritable bowel syndrome (IBS), lactose intolerance, and ulcerative colitis.
During a physical exam, a physician will check for bloating, swelling, and painful or tender spots in your abdomen.
Additional tests are often needed to diagnose Crohn’s disease and may include: blood tests, stool tests, colonoscopy, upper GI (gastrointestinal) endoscopy, wireless capsule endoscopy, and imaging tests like X-rays and computerized tomography (CT) scans.
Learn More About Crohn’s Disease Symptoms and Diagnosis
Duration of Crohn’s Disease Flares
A period of time in which symptoms of Crohn’s are severe is called a flare. The length of a flare varies widely from person to person, but generally, can last anywhere from a couple of days to several months.
If a flare is left untreated, it can cause lasting complications and permanent damage, so it’s important to work with your doctor on a treatment plan.
For an individual with Crohn’s a period of time with no symptoms is called remission, which can last for several days, weeks, and even years.
The goal of treatment for Crohn’s disease is to achieve and maintain remission.
Learn More About Crohn’s Disease Flares
Treatment and Medication Options for Crohn’s Disease
Treatment for Crohn’s disease usually involves a number of different drugs.
Some of these drugs are meant to prevent flares of your disease — periods in which your symptoms return or worsen. Others are prescribed to reduce inflammation and treat symptoms when a flare takes place.
You may also be prescribed antibiotics to treat symptoms or complications due to a bacterial infection.
For most people with Crohn’s disease, a time will come when medication alone won’t be enough, and surgery will be required.
Surgical treatments may include removing a diseased area of the intestines, opening a narrowed or blocked area, or even removing the entire colon.
Most surgical treatments allow people with Crohn’s to live symptom-free for a number of years.
Alternative therapies can also help to reduce symptoms and maintain remission. Research shows that supplements like probiotics can reduce the duration of flares.
Learn More About Treatments for Crohn's Disease
How Can Your Diet Affect Crohn’s Disease?
There’s no single diet that helps all people with Crohn’s disease.
You may find that making certain dietary changes helps reduce uncomfortable symptoms during flares, such as bloating, gas, and diarrhea.
Foods that commonly trigger symptoms include certain whole grains, nuts and seeds, raw fruits and vegetables, spicy foods, fatty or greasy foods, dairy products, and caffeinated or alcoholic beverages.
If you experience malnutrition due to Crohn’s disease, you may also need to focus on getting enough of certain nutrients in your diet.
When your symptoms are at their worst, it’s often helpful to focus on easy to digest meals and snacks.
Learn More About Diet For Crohn's Disease
Research and Statistics: How Many People Have Crohn's Disease?
Studies show that the condition has become more common in the United States and certain other countries, for reasons that aren't fully understood.
Men and women are equally likely to be affected.
Related Conditions and Causes of Crohn’s Disease
Crohn’s is a form of irritable bowel disease, an umbrella term used to describe disorders that involve chronic inflammation of the digestive tract. The other main type of IBD is ulcerative colitis, a condition characterized by chronic inflammation and ulcers in the lining of the colon and rectum.
It’s also important not to confuse an irritable bowel disease like Crohn’s or ulcerative colitis with irritable bowel syndrome (IBS). The two conditions sound similar and even share some of the same symptoms but are very different.
While scientists are working to better understand the exact cause of IBD, it’s generally believed that the body mistakes normal bacteria in the gut for an enemy. As a result of the body’s natural defenses, this causes chronic inflammation of the digestive tract. In contrast, there are no physical changes to the digestive system with IBS.
Crohn’s and COVID-19
The coronavirus pandemic has forced everyone to take extra precautions when it comes to health and safety. This is especially true for individuals with a compromised immune system. Although research shows that people living with Crohn’s disease are no more susceptible to catching the virus than the general population, organizations including the American College of Gastroenterology and the Crohn’s and Colitis Foundation have issued a number of new guidelines to help limit the spread of the infection.
And, doctors recommend that people with inflammatory bowel diseases receive the COVID-19 vaccine. Talk to your doctor to see if you also need a COVID-19 booster shot.
There are a number of resources available to help people with Crohn’s manage these difficult times — from medication assistance to telehealth appointments to virtual therapy for mental health.
Learn More About Crohn’s and COVID-19
Additional reporting by Jordan M. Davidson.


Editorial Sources and Fact-Checking
- Definition and Facts for Crohn's Disease. National Institute of Diabetes and Digestive and Kidney Diseases. September 2017.
- Genetics Initiative. Crohn’s and Colitis Foundation.
- Learning About Crohn’s Disease. National Human Genome Research Institute. September 27, 2011.
- Types of Crohn’s Disease and Associated Symptoms. Crohn’s and Colitis Foundation.
- Causes of Crohn's Disease. Crohn's and Colitis Foundation.
- Overview of Crohn's Disease. Crohn's and Colitis Foundation.
- Crohn's Disease — Causes. MedlinePlus. August 18, 2020.