Some people who sleepwalk perform complex behaviors while asleep, such as driving.
Formally known as somnambulism, sleepwalking is a sleep disorder in which a person gets out of bed and walks around, or performs other activities, while still sleeping or in a sleeplike state.
Sleep is divided into two distinct states: rapid-eye movement (REM), during which vivid dreams occur, and non-rapid eye movement (NREM).
NREM is further divided into three stages associated with different electrical activities in the brain and deepness of sleep.
Each night, you go through several cycles of REM and NREM sleep.
Sleepwalking most often occurs during the deepest NREM sleep stage — known as N3, or slow-wave sleep.
It can also occur during N2, or light sleep, according to a 2013 review in The Lancet Neurology.
Why Do People Sleepwalk?
It's unclear what exactly causes people to sleepwalk.
Sleepwalking has long been thought of as a disorder of arousal, in which certain parts of the brain don't fully activate after NREM — causing a person to be stuck between being fully asleep and fully awake.
Another theory holds that sleepwalking may be the result of a dysfunction in slow-wave-sleep regulation.
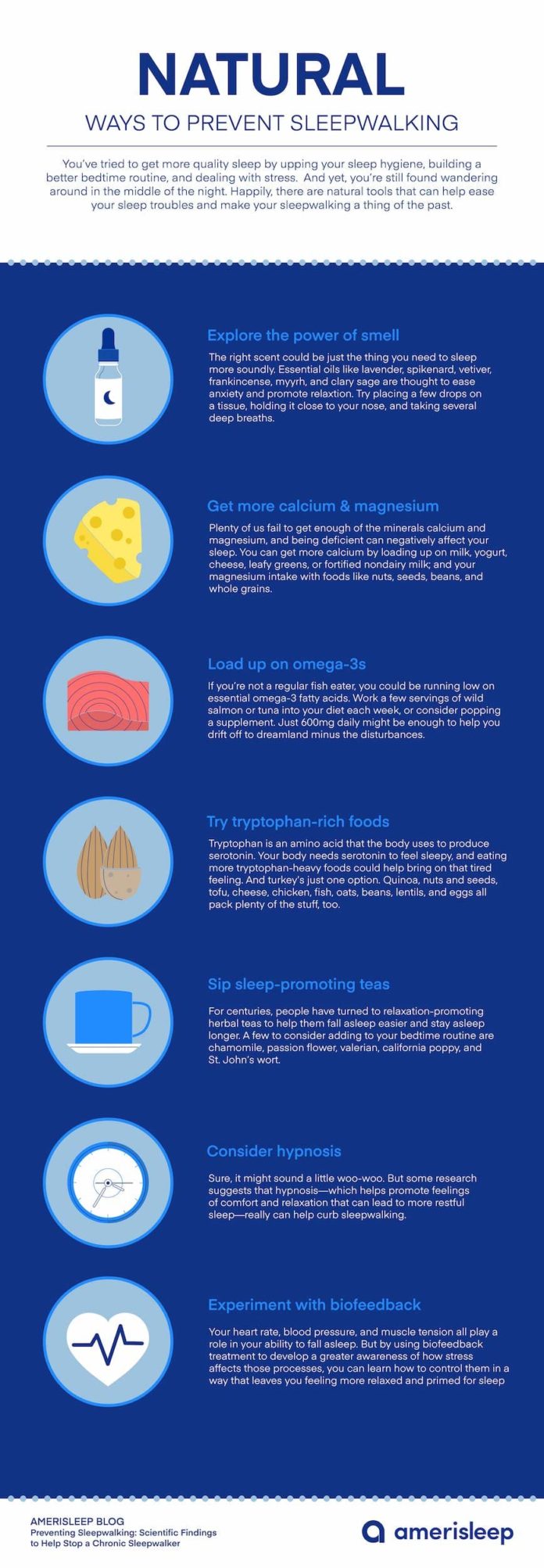
Whatever the case, there are many factors that can contribute to sleepwalking, including:
- Various stimulant and depressant medications, such as lithium, Ambien (zolpidem tartrate), and Wellbutrin or Zyban (bupropion)
- Sleep deprivation
- Alcohol consumption
- Airway disorders, such as obstructive sleep apnea
- Psychological disturbances, such as stress, anxiety, or depression
- Childhood trauma
- Migraine headaches
- Other sleep disorders, such as narcolepsy and restless legs syndrome
- Certain medical conditions, such as hyperthyroidism, head injury, gastroesophageal reflux disease (GERD), and stroke
- Travel
Sleepwalking also appears to run in families.
About 80 percent of adult sleepwalkers have at least one family member who also sleepwalks, and sleepwalking is more common in children with a parent who has a history of it, according to The Lancet Neurology report.
Sleepwalking Prevalence
Sleepwalking is more common in children, most likely because people experience less N3 sleep as they grow older, according to the National Institutes of Health.
According to The Lancet Neurology review, the prevalence of sleepwalking rises and falls throughout childhood. Sleepwalking affects:
- About 3 percent of toddlers between 2.5 and 4 years old
- About 11 percent of 7- to 8-year-olds
- About 13.5 percent of 10-year-olds
- About 12.7 percent of 12-year-olds
The rate of sleepwalking then rapidly drops in adolescence. Only about 2 to 4 percent of adults sleepwalk.
Signs and Symptoms of Sleepwalking
Sleepwalking often occurs soon after a person goes to sleep, usually within one to two hours. Even though the condition is called "sleepwalking," people often engage in numerous other types of behavior.
Sometimes these behaviors are simple, such as gesturing or pointing at a wall, or talking. But certain behaviors can be more complex.
These behaviors can include:
- Getting dressed
- Cooking or preparing a snack
- Driving a vehicle
- Playing a musical instrument
- Engaging in sexual activity (this is sometimes considered a separate issue distinct from sleepwalking, called sexsomnia)
- Engaging in unusual activities, such as urinating in a closet (generally occurs in children)
- Engaging in dangerous activities, such as jumping out a window
People who sleepwalk may also exhibit other symptoms during or after an episode, such as:
- Sitting up in bed and opening their eyes, often with a glazed-over expression or blank look on their face
- Confusion or disorientation after waking up
- Amnesia of the sleepwalking episode (partial or total loss of memory)
- Difficulty arousing from sleepwalking
- Being aggressive after being woken up
Research also suggests that sleepwalking can cause excessive sleepiness or drowsiness during the day.
How Is Sleepwalking Diagnosed?
Getting a diagnosis of sleepwalking from a healthcare professional usually isn't necessary, because it's likely you'll notice your behavior on your own (unless you live alone and are completely unaware of your nighttime habits).
But your doctor may give you a physical or psychological exam to rule out other possible causes of your behavior.
Certain conditions, such as REM-sleep behavior disorder and nocturnal frontal lobe epilepsy, can cause complex sleep behaviors that may appear similar to sleepwalking.
In some cases, a sleep study (polysomnogram) — in which you spend a night in a sleep lab, where technicians take physiological measurements while you sleep — may be required for an accurate diagnosis.
Treatment and Medication Options for Sleepwalking
Treatment generally isn't necessary for occasional sleepwalking. But your doctor may suggest treatment if your condition is resulting in disturbing or dangerous behaviors.
Treatment may involve:
- Correcting the underlying cause of sleepwalking, such as sleep deprivation or a medical condition
- Anticipatory awakenings, in which you're awoken shortly before the time you normally start to sleepwalk
- Sedative medication in the benzodiazepine class, such as Valium (diazepam), Klonopin (clonazepam), or Tofranil (imipramine)
- Hypnosis


Editorial Sources and Fact-Checking
- A. Zadra, A. Desautels, D. Petit, and J. Montplaisir (2013). "Somnambulism: clinical aspects and pathophysiological hypotheses." The Lancet Neurology.
- John R. Hughes (2007). "A review of sleepwalking (somnambulism): The enigma of neurophysiology and polysomnography with differential diagnosis of complex partial seizures." Epilepsy and Behavior.
- Sleepwalking; National Sleep Foundation.
- Sleepwalking; MedlinePlus.
- Sleepwalking & Sleep Talking; American Academy of Sleep Medicine.
- Sleepwalking; Mayo Clinic.