Hepatitis is an inflammation of the liver, and hepatitis C is liver inflammation caused by the hepatitis C virus (HCV).
Though these genotypes appear to affect people similarly, they respond differently to treatments, and it's possible to be infected with more than one HCV genotype at the same time.
Whatever the genotype, hepatitis C is considered either acute (clears up within six months) or chronic (lasts more than six months).
Signs and Symptoms of Hepatitis C
- Jaundice
- Fatigue
- Fever
- Dark urine
- Gastrointestinal issues
- Loss of appetite
- Joint pain
- Weight loss
People with chronic hepatitis C, on the other hand, often don’t show any symptoms until the liver becomes damaged, which could be years after exposure.
Learn More About Signs and Symptoms of Hepatitis C
Causes and Risk Factors of Hepatitis C
Hepatitis C is transmitted when the blood of an infected person enters the body of someone who isn't infected.
Before 1992, when widespread screening of the blood supply began, people could contract the virus through blood transfusions and organ transplants.
Today, the most common ways that transmission occurs are:
- Through the sharing of needles and syringes for intravenous drug use
- Through accidental needle injuries in healthcare settings
- During birth, if the mother has hepatitis C
Using personal care items — including razors and toothbrushes — that have come in contact with blood infected with HCV can put you at risk of hepatitis C.
"Hepatitis C can be easily transmitted with any blood-to-blood contact (much more easily than HIV)," Dr. Malvestutto says. "There have been cases of transmission through sharing of razors or sharing 'straws' to inhale drugs nasally."
Though less common, it's also possible to acquire a hepatitis C infection by having unprotected sex with someone who has the virus.
Given that hepatitis C is spread through blood contact, an infected mother cannot give her baby hepatitis C through breastfeeding and you cannot contract the virus through saliva (kissing).
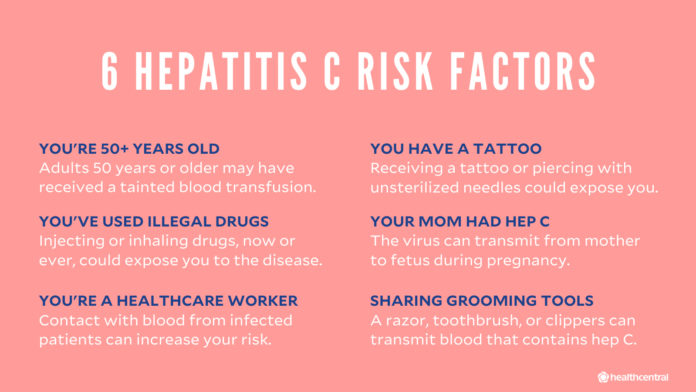
Some factors that increase your risk of hepatitis C:
- Working in the healthcare setting or another field in which you have regular contact with blood
- Having HIV (About 21 percent of people with HIV also have hepatitis C, notes the CDC.
- Receiving a tattoo or piercing with nonsterile instruments
- Undergoing dialysis for many years
Hepatitis C has some surprising ways of showing up. For example, your birth date alone may put you at a higher risk. Healthcare professionals and members of the military are also at greater risk.
Learn More About Causes and Common Risk Factors of Hepatitis C
How Is Hepatitis C Diagnosed?
In addition to taking your medical history and performing a physical exam to look for signs of liver damage, your doctor will use the results of certain blood tests to make a diagnosis.
An initial blood test screens for HCV antibodies — proteins your body produces in reaction to the presence of the hepatitis virus. If the result is negative, it means you’ve never had HCV in your blood. If the result is positive, you were exposed to HCV at some point.
If the antibody test is positive, your doctor will conduct another blood test that looks for the RNA (genetic material) of HCV in your blood. There are qualitative HCV RNA tests and quantitative ones. A qualitative test determines the presence or absence of the virus in your body, while the quantitative RNA test measures the viral load, or how much virus is in the blood.
Another blood test will also be used to determine which genotype (or genotypes) of HCV you have, as that will affect your treatment plan.
Your doctor may conduct other blood tests to assess liver damage.
Prognosis of Hepatitis C
Duration of Hepatitis C
The other 75 to 85 percent of people go on to become hepatitis C carriers and develop a chronic infection, which can last a lifetime if left untreated. Chronic hepatitis C can lead to hepatitis C–related complications, including chronic liver disease, cirrhosis, and liver cancer.
Treatment and Medication Options for Hepatitis C
The last few years have seen extraordinary advances in the treatment of hepatitis C.
For decades, the standard treatment was a combination antiviral therapy consisting of a pegylated interferon (a synthetic version of a protein secreted by immune system cells in response to pathogens) and ribavirin, sometimes called PEG-riba therapy. This involved weekly injections of the pegylated interferons along with twice-daily oral doses of ribavirin. Sometimes interferon was prescribed without ribavirin.
The treatment by interferon lasted six months to a year, and cured only 40 to 50 percent of hepatitis C patients. The painful injections often made patients feel ill with flu-like symptoms.
But now, hepatitis C can be treated with a number of direct-acting antiviral pills that act faster and much more effectively than the older interferon treatment. These combination oral medicines have 90 to 100 percent cure rates, and they work in weeks instead of months. Some of these drugs may be used in combination with ribavirin.
Medication Options
The choice of medication and length of treatment depends on which genotype of the virus a patient has, how much liver damage they’ve sustained, and whether they’ve already been treated for hepatitis C. Medication options include:
- Simeprevir
- Sofosbuvir
- Harvoni (ledipasvir and sofosbuvir)
- Viekira Pak (ombitasvir, paritaprevir, dasabuvir, and ritonavir)
- Daklinza (daclatasvir and sofosbuvir)
- Technivie (ombitasvir, paritaprevir, and ritonavir)
- Zepatier (elbasvir and grazoprevir)
- Epclusa (sofosbuvir and velpatasvir)
- Vosevi (sofosbuvir, velpatasvir, and voxilaprevir)
- Mavyret (glecaprevir and pibrentasvir)
People with hepatitis C should avoid alcohol, as it can damage the liver. Check with your doctor before taking any medication or supplements that might also damage the liver. If liver damage is present, the CDC recommends asking your doctor about getting vaccinated against hepatitis A and hepatitis B. A vaccine for hepatitis C is not yet available.
If HCV-related cirrhosis has led to liver failure, a liver transplant is the only real treatment.
Learn More About How Hepatitis C Is Treated
Alternative and Complementary Therapies
- Milk thistle
- Vitamin D
- SNMC (Stronger Neominophagen C)
- CH100 (Cathy Herbal Tablet)
- Thymus extracts
Learn More About Alternative and Complementary Therapies for Hepatitis C
Prevention of Hepatitis C
There is no vaccine for hepatitis C.
The best way to avoid getting hepatitis C is to reduce your risk factors, such as by:
- Not using intravenous drugs
- Using only sterile injection equipment if you do inject drugs, and not reusing or sharing your equipment
- Not sharing personal care items that might have blood on them, including razors, toothbrushes, and nail clippers
- Safely handling needles and other sharp equipment if you are a healthcare worker
- Not getting a tattoo, body piercing, or acupuncture treatment from an unlicensed practitioner
- Practicing safe sex
Complications of Hepatitis C
According to the CDC, 10 to 20 percent of people with HCV develop cirrhosis — irreversible scarring of the liver that prevents the organ from functioning as it should — over a period of two to three decades.
People with cirrhosis have an increased risk for liver cancer.
- Buildup of fluid in the abdomen, feet, ankles, or legs
- Enlarged spleen
- Enlarged blood vessels in the esophagus and stomach, which are more susceptible to tear and cause internal bleeding
Cirrhosis can eventually lead to end-stage liver disease, or liver failure, which is accompanied by several debilitating symptoms, including a buildup of toxins in the brain that can result in cognitive decline and coma. Cirrhosis also increases the risk for liver cancer.
"Unfortunately, HCV can destroy the liver and cause a horrendous death," says Andrea Branch, PhD, a professor of medicine and liver diseases at the Icahn School of Medicine at Mount Sinai in New York City. "To get the maximum benefit of treatment, it is important to treat HCV as soon as the infection is diagnosed."
Learn More About the Complications of Hepatitis C: How It Affects Your Body in the Short and Long Term
Research and Statistics: Who Has Hepatitis C? How Many People Have Hepatitis C?
Health officials reported 2,967 cases of acute hepatitis C in 2016, but the CDC estimates that the actual number of acute cases is 13.9 times the number of reported cases in any year. The CDC put the real number of acute hepatitis C cases in 2016 at an estimated 41,200.
Despite these estimates, "we really do not know how many people are infected with HCV," Dr. Branch says, adding that the U.S. estimates come from specific datasets that "do not include prisoners or the homeless and have too small a sample size to yield precise data."
It's unclear how many people fail to get treatment in time and die from HCV-related issues. According to the CDC, there were 18,153 reported deaths related to HCV, but this is likely an underestimate.
"HCV may be causing 3 to 5 times more deaths than we know," Branch says. "Better information about the number of HCV-related deaths would help make HCV testing and treatment more of a priority."
Resources We Love
Favorite Orgs for Essential Hep C Info
Hepatitis C Association
This organization is dedicated to educating the public about all aspects of the hepatitis C virus. The site presents the latest hep C news and events, as well as resources for those without insurance. The association is the managing partner for the Help4Hep toll-free support and resource line at 877-435-7443.
Hepatitis Foundation International
We like the foundation’s dedication to promoting healthy living habits for people with hep C, especially those that can benefit the liver. The group produced the DVD Live-R-Die to educate young adults about binge drinking, drug abuse, and other liver-damaging behaviors.
American Liver Foundation
The viral infection hep C can take its toll on the liver. This foundation supports education, advocacy, and research for the prevention of liver disease. It has a nationwide network of offices ready to help individuals with any related questions.
United Network for Organ Sharing
One of the most common reasons for liver transplantation in the United States is organ failure due to hep C. This network serves as a comprehensive resource for those exploring liver transplant options, organ donation, and medical advances. Profiles of people who have had transplants and connections to support groups are available.
Favorite Hep C Financial Resources
NeedyMeds
This nonprofit devotes its energies to help people afford healthcare and medication. It offers a free drug discount card that extends a discount of up to 80 percent at more than 65,000 pharmacies nationwide. Anyone (and their family and friends) can use the card regardless of income level or insurance status.
RxAssist
RxAssist guides people to free or low-cost medicine programs. Visitors to the website can type a drug's name into the search tool to find patient assistance programs that can help with costs. The group also gives a wealth of information on various drug discount cards.
Partnership for Prescription Assistance
Plug the name of a drug into this free service and it searches for patient assistance programs that will help pay for the medication. It also has a great tool to help find free or low-cost clinics near you.
Patient Advocate Foundation Co-Pay Relief
Those who qualify can get awards of up to $15,000 a year to pay for hep C treatment. Eligibility requirements include an income below 400 percent of the federal poverty guidelines. In addition, the foundation presents links to other financial resources and pharmaceutical assistance programs.
Favorite Hep C Alternative Medicine Resource
National Center for Complementary and Integrative Health (NCCIH)
Although hep C can be successfully treated with modern medicine, many people turn to dietary supplements with the goal of curing their illness. The most commonly used is silymarin (milk thistle). Although the NCCIH says that no supplement is effective for hep C, the center provides the latest scientific data on a range of products, including probiotics, zinc, licorice root, and colloidal silver.
Favorite Hep C Support Networks
Hepatitis Central
This site gives a very detailed listing of live hep C support groups in cities across the country. Meetings are often for those undergoing treatment or people who have questions about treatment. A database that searches by ZIP code makes it simple to find a support group near you.
+supportgroups
This online support network has about 34,000 members at latest count. People can anonymously post about all concerns related to the disease, including issues about stigma, depression, and care.
Favorite Hep C Online Magazine and Blogs
Hep Mag
Hep Mag publishes current articles about people living with hep C, plus it offers a forum for people to ask questions and share stories and information with other readers. The online magazine also features a blog on funding, cures, liver disease, and related matters.
Feedspot
Feedspot, a feed compiling news from online sources, lists 20 top blogs and websites to explore concerning hepatitis C. Readers can connect with one another and find out about the latest drug research developments.
Favorite Hep C App
HepCure
This web-based app for people infected with the hepatitis C virus offers health management, decision support, and regular educational webinars. Developed in part by the Icahn School of Medicine at Mount Sinai in New York City, the app also gives providers a way to track their hep C patients.
Favorite Sites for Hep C Products
Hep C can now be cured with an 8- to 12-week course of medication. The pharmaceutical companies that produce these drugs all present useful information and, in some cases, details on how to get the medication at a lower cost. Here are the latest hep C drugs approved by the FDA:
- Mavyret (glecaprevir and pibrentasvir)
- Vosevi (sofosbuvir, velpatasvir, and voxilaprevir)
- Epclusa (sofosbuvir and velpatasvir)
- Zepatir (elbasvir and grazoprevir)
- Harvoni (ledipasvir and sofosbuvir)
Additional reporting by Laura McArdle.


Editorial Sources and Fact-Checking
- Hepatitis C. San Francisco Department of Public Health.
- Murphy DG, Sablon E, Chamberland J, et al. Hepatitis C Virus Genotype 7, a New Genotype Originating from Central Africa. Journal of Clinical Microbiology. December 2014.
- Borgia SM, Hedskog C, Parhy B, et al. Identification of a Novel Hepatitis C Virus Genotype From Punjab, India: Expanding Classification of Hepatitis C Virus Into 8 Genotypes. Journal of Infectious Diseases. June 2018.
- Hepatitis C FAQs for the Public: Overview. Centers for Disease Control and Prevention. April 23, 2018.
- Hepatitis C FAQs for Health Professionals: Overview and Statistics. Centers for Disease Control and Prevention. April 30, 2018.
- Hepatitis B FAQs for the Public: Transmission. Centers for Disease Control and Prevention. April 20, 2018.
- Hepatitis C. National Institute of Diabetes and Digestive and Kidney Diseases. May 2017.
- Hepatitis C Treatments Give Patients More Options. U.S. Food and Drug Administration. May 4, 2017.
- Hepatitis C and Dietary Supplements. National Center for Complementary and Integrative Health. June 24, 2019.
- Complementary and Integrated Medicine for Hepatitis C. U.S. Department of Veterans Affairs.
- Halegoua-De Marzio DL, Fenkel JM. Complementary and Alternative Medications in Hepatitis C Infection. World Journal of Hepatology. January 2014.
- Definition and Facts for Cirrhosis. National Institute of Diabetes and Digestive and Kidney Diseases. March 2018.
- Hepatitis C Factsheet. World Health Organization. October 2, 2017.
- CDC Now Recommends All Baby Boomers Receive One-Time Hepatitis C Test. Centers for Disease Control and Prevention. August 16, 2012.
- New Hepatitis C Infections Nearly Tripled Over Five Years. Centers for Disease Control and Prevention. May 11, 2017.
- Bakr I, Rekacewicz C, El Hosseiny M, et al. Higher Clearance of Hepatitis C Virus Infection in Females Compared with Males. Gut. August 2006.
- Wang CC, Krantz E, Klarquist J, et al. Acute Hepatitis C in a Contemporary US Cohort: Modes of Acquisition and Factors Influencing Viral Clearance. The Journal of Infectious Diseases. November 2007.
- Baden R, Rockstroh J, Buti M. Natural History and Management of Hepatitis C: Does Sex Play a Role? The Journal of Infectious Diseases. July 2014.
- Alcoholic Hepatitis. Mayo Clinic. March 27, 2018.
- Autoimmune Hepatitis. National Institute of Diabetes and Digestive and Kidney Diseases. March 2014.
- Drug-Induced Liver Injury. Medline Plus. April 30, 2018.
- What to Know About Liver Disease and COVID-19. Centers for Disease Control and Prevention. February 8, 2021.
- Wang Q, Davis PB, Xu R. COVID-19 Risk, Disparities, and Outcomes in Patients With Chronic Liver Disease in the United States. EClinicalMedicine. December 22, 2020.