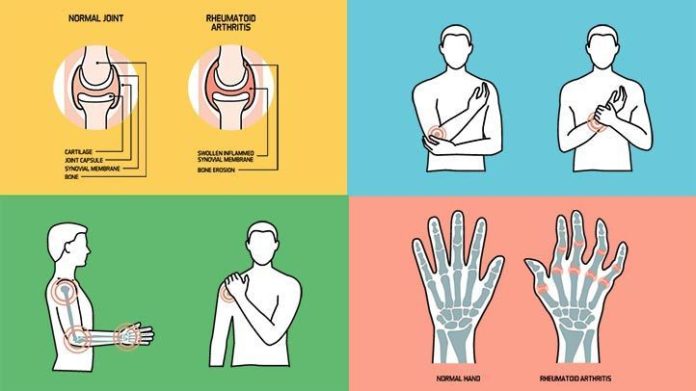
Rheumatoid arthritis (RA) is a chronic inflammatory disease of the joints. Within the body, joints are the points where bones come together and allow for movement. Most of these joints — those called synovial joints — also provide shock absorption.
RA is an autoimmune condition, in which your immune system mistakes the linings of your joints as "foreign" and attacks and damages them, resulting in inflammation and pain.
Signs and Symptoms of Rheumatoid Arthritis
Rheumatoid arthritis is a complex disease that is not well understood by medical practitioners or researchers.
If you're experiencing RA symptoms, it's crucial to get diagnosed as soon as possible so that you can receive prompt treatment.
Learn More About Rheumatoid Arthritis Signs and Symptoms
Causes and Risk Factors of Rheumatoid Arthritis
RA develops when white blood cells, which normally protect the body from foreign invaders such as bacteria and viruses, enter the synovium (the thin tissue that lines the synovial joints). Inflammation ensues — the synovium thickens, causing swelling, redness, warmth, and pain in the synovial joint.
Researchers don't know exactly what causes the immune system to invade the synovium, but it's believed that genes and environmental factors play a role in the development of RA.
But not everyone with these identified gene variants develops RA, and people without them can still develop it. So, it's likely that environmental factors often trigger the disease, particularly in people with a genetic makeup that makes them more susceptible to it. These factors include:
- Viruses and bacteria (though certain infections may reduce RA risk, at least temporarily)
- Female hormones
- Exposure to certain kinds of dust and fibers
- Exposure to secondhand smoke
- Obesity, which also increases progression of disability for people with RA.Obese patients are less likely to achieve RA remission regardless of the treatment they receive.
- Severely stressful events
- Foods
Children up to age 16 who experience prolonged swollen or painful joints anywhere in the body are typically diagnosed with juvenile idiopathic arthritis (JIA).
Learn More About Juvenile Idiopathic Arthritis: Symptoms, Causes, Diagnosis, and Treatment
Duration of Rheumatoid Arthritis
But remission doesn't happen for everyone, and because the pain and other symptoms of RA may change over time, pain management can be an ongoing concern. In addition to pain medications like nonsteroidal anti-inflammatory drugs and corticosteroids, there are many options for pain relief for people living with RA. These include, among others:
- Fish oil supplements
- Hot and cold treatments
- Exercise and movement
- Mind-body modalities such as mindfulness-based stress reduction and acceptance and commitment therapy
- Biofeedback
Learn More About How Rheumatoid Arthritis Progresses
Treatment and Medication Options for Rheumatoid Arthritis
To treat RA, doctors aim to stop the progression of the disease by reducing symptoms, controlling inflammation, minimizing joint and organ damage, and improving physical function.
Proven treatments include medication and physical therapy. Early, aggressive measures can help control symptoms and complications before the disease significantly worsens, by reducing or altogether stopping inflammation as quickly as possible.
Medication Options
In recent years, there have been significant advancements in medicines for treating RA, but there is still no cure. Medications known as disease-modifying antirheumatic drugs (DMARDs) are considered the gold standard for RA treatment.
In general, these drugs work by slowing the inflammation and protecting the joints from further damage, and are generally prescribed shortly after diagnosis. The type of DMARD a doctor prescribes depends on several factors, including disease severity and the balance between the medication's benefits and potential side effects.
Biologics and JAK inhibitors are newer options alongside traditional DMARDs. Traditional DMARDs target the entire immune system, while biologics work by targeting specific steps in the inflammatory process, and JAK inhibitors block action in your body to help prevent the inflammation before it starts. Traditional DMARDs are usually taken in pill form, as are JAK inhibitors; biologics are typically injected or delivered via an intravenous infusion.
RELATED: New Medication Guidelines for Treating Rheumatoid Arthritis Released
Learn More About Rheumatoid Arthritis Medications
Alternative and Complementary Therapies for Rheumatoid Arthritis
Certain lifestyle changes and home remedies may be beneficial — in addition to the conventional treatment of medication, physical therapy, and surgery — if needed.
Relaxation techniques, visualization exercises, group counseling, and psychotherapy can help reduce the stress of living with RA. Sleeping well is also an important part of managing symptoms.
You should always check with your medical provider before trying any complementary or alternative therapies.
Learn More About Alternative Therapies for Rheumatoid Arthritis
Many people can manage RA with medication and physical therapy, but joint surgery may be an option if your joint damage is severe and limiting your quality of life.
Learn More About Treatment for Rheumatoid Arthritis: Medications, Alternative and Complementary Therapies, Surgery Options, and More
Complications of Rheumatoid Arthritis
It's well established that rheumatic diseases such as RA increase the risks for developing a variety of health conditions.
The most common RA comorbidity is cardiovascular disease, but the condition is also associated with several specific cardiovascular issues, including heart attack, stroke, congestive heart failure, peripheral vascular disease, and atherosclerosis.
RA can also lead to inflammation in other areas of the body, including blood vessels, where it's known as rheumatoid vasculitis; the lungs, resulting in rheumatoid lung disease or other conditions; the eyes; and the wrists, causing carpal tunnel syndrome.
Learn More About the Complications of Rheumatoid Arthritis: How It Affects Your Body in the Short and Long Term
Dietary Modifications to Consider for Rheumatoid Arthritis
While there is a lot of interest in the role of diet and nutrition in symptom management for rheumatoid arthritis, there is no comprehensive research on the topic nor is there a dietary magic formula to fight RA symptoms.
But some evidence suggests that eating certain foods may help reduce inflammation and improve symptoms for some people, while other foods have been shown to worsen inflammation and related symptoms.
For instance, the ketogenic diet — which is high in fats that promote inflammation and low in certain healthy grains, fruits, and vegetables that help fight inflammation — is generally believed to be bad for RA symptoms and pain.
Learn More About Rheumatoid Arthritis and Diet
Research and Statistics: Who Has Rheumatoid Arthritis?
Resources We Love
Favorite Orgs for Essential Rheumatoid Arthritis Information
The American College of Rheumatology is an organization for physicians, health professionals, and scientists that advances rheumatology through education, research, advocacy, and practice support relating to the care of people with arthritis and rheumatic and musculoskeletal diseases. It publishes two medical journals (Arthritis & Rheumatology and Arthritis Care & Research) and promotes research into rheumatological conditions.
The Arthritis Foundation is a nonprofit organization dedicated to the prevention, control, and cure of arthritis. The foundation provides information and resources, access to optimal care, advancements in science, and community networking.
CreakyJoints is a leading support, education, advocacy, and research organization for people living with arthritis and rheumatic disease. It is dedicated to raising awareness of all forms of arthritis, which includes educating people about the available varieties of treatment and management strategies.
Favorite Online Support Network for RA
The Live Yes! Arthritis Network, from the Arthritis Foundation, provides a network of support with the aim of helping people live their best lives. By exchanging ideas, tips, and experiences with others in provided online forums covering a variety of topics, the network empowers people with RA to gain confidence in dealing with their disease proactively.
Favorite Apps, Products, and Gadgets
Arthritis Power App
CreakyJoints has partnered with rheumatology researchers at the University of Alabama at Birmingham to create this useful app that helps you track your symptoms and medications and share your experiences of living with RA. In addition to RA, the app also includes research for conditions such as ankylosing spondylitis; psoriatic arthritis; psoriasis; osteoporosis, osteopenia, and low bone mineral density; osteoarthritis; fibromyalgia; gout; juvenile idiopathic arthritis; inflammatory bowel diseases, like Crohn’s and ulcerative colitis; lupus; scleroderma (systemic sclerosis); polymyositis; and dermatomyositis.
Dycem Super Grip Tape, $13.95
Dycem's self-adhering Super Grip Tape provides a cushioned grip that feels more comfortable on the hands. The tape adheres to a variety of surfaces, including brooms, wheelchair arms, mobility devices, and even pens and cutlery. The nonslip grip will help increase the friction of any surface you grab.
Besmon Electric Jar Opener, $22.99
This jar opener can handle any jar with lids that are 1 to 3.5 inches in diameter. It’s recommended for people with arthritis, to save your joints the strain of twisting stubborn lids.
Hamilton Beach Smooth Touch Electric Can Opener $31.85
The Smooth Touch can open both pop-top and regular cans. It is designed so that it cuts along the side of the can and not the top, minimizing the blade's contact with food, preventing splashing, and creating a smooth, touchable lid.
IMAK Compression Arthritis Gloves, $20.99
Many people with rheumatoid arthritis consider compression gloves a must-have accessory. According to research published in Therapeutic Advances in Musculoskeletal Disease, hand symptoms including pain, stiffness, and swelling improve greatly with the use of compression gloves. IMAK remains one of the easiest brands of gloves to find, both online and in stores.
Sunbeam Warming Blanket
Sunbeam's electric blanket can help those with arthritis get off to a better start in the morning by providing the heat necessary to loosen stiff joints. An easy-to-use controller can adjust the blanket through 10 heating levels to help you warm up your joints before getting out of bed. The blanket comes in twin, full, queen, and king sizes to fit all standard-size beds.
Favorite Patient Blogs
Chronic Eileen
Over a period of two and a half years, Eileen Davidson was diagnosed with rheumatoid arthritis, osteoarthritis, and fibromyalgia. She began writing Chronic Eileen in June 2017 as a way to battle her struggles with progressing anxiety and depression and to help her handle her new role as a mother with a chronic illness (her article on parenting techniques is definitely worth a read). Her posts share many of these ideas, such as whether arthritis will make tattoos hurt or how to calm the “bitch within” when living with a chronic illness.
Carla’s Corner
With 25 years of corporate communications experience, Carla Kienast has focused her messaging skill on helping others living with rheumatoid arthritis through her blog. Diagnosed with RA in 2008, Kienast has been through 19 surgeries, including three joint replacements, two spinal fusions, and two rotator cuff operations. She describes her extraordinary experiences dealing with hip and shoulder surgeries, and covers her various, and sometimes ineffective, drug treatments, all with a sense of humor.
From This Point. Forward.
Mariah Leach was diagnosed with rheumatoid arthritis at age 25 while pursuing dual graduate degrees. Since then, she has undoubtedly made the most of living with a chronic illness, including giving birth to her third child. In addition to her blog, Leach writes for various health websites. On Mamas Facing Forward, she pays special attention to mothers living with RA in articles on sex, parenting, treatment, and ordinary life with RA.
RELATED: 10 Arthritis Blogs to Watch in 2020
Favorite Annual Meetings
American College of Rheumatology Annual Meeting
Every year, nearly 16,000 rheumatologists, rheumatology health professionals, fellows in training, patient advocates, and exhibitors from more than 100 countries gather to discuss the latest scientific advances and clinical issues surrounding rheumatoid arthritis. In 2021, it will be held virtually, due to COVID-19. The annual convention hosts sessions that provide ample opportunity for professional development, networking, and access to the latest rheumatology research and clinical applications.
Rheumatoid Arthritis and COVID-19
As the novel coronavirus persists, you know you must take extra precautions to protect your health. Find the latest, most accurate information in our guide.
Learn More: A Guide to Living With RA During the COVID-19 Pandemic: Help, Resources, and Making a Personal Checklist
RELATED: 8 Things People With Rheumatoid Arthritis Must Know About the COVID-19 Vaccines
Editorial Sources and Fact-Checking
- Rheumatoid Arthritis (RA). Centers for Disease Control and Prevention. July 27, 2020.
- Rheumatoid Arthritis: Causes, Symptoms, Treatments, and More. Arthritis Foundation.
- Patient Education: Rheumatoid Arthritis Symptoms and Diagnosis (Beyond the Basics). UpToDate. July 2021.
- Rheumatoid Arthritis: When Your Immune System Attacks Your Body. NIH MedlinePlus. Summer 2014.
- Rheumatoid Arthritis. MedlinePlus. August 18, 2020.
- Dedmon LE. The Genetics of Rheumatoid Arthritis. Rheumatology. October 2020.
- Nguyen Y, Salliot C, Mariette X, et al. Association Between Passive Smoking in Childhood and Adulthood, and Rheumatoid Arthritis: Results from the French E3N-EPIC Cohort Study. Annals of the Rheumatic Diseases. May 19, 2021.
- Baker JF, England BR, Mikuls TR, et al. Obesity, Weight Loss, and Progression of Disability in Rheumatoid Arthritis. Arthritis Care & Research. April 2018.
- Abuhelwa AY, et al. Association Between Obesity and Remission in Rheumatoid Arthritis Patients Treated with Disease-Modifying Anti-Rheumatic Drugs. Scientific Reports. October 2020.
- Rheumatoid Arthritis Causes. NHS. August 28, 2019.
- What “Type” of RA Do You Have? Arthritis Foundation.
- Rheumatoid Arthritis. Johns Hopkins Arthritis Center.
- Why Your RA Went Into Remission, but Relapsed. Arthritis Foundation.
- Patient Education: Rheumatoid Arthritis Treatment (Beyond the Basics). UpToDate. July 2021.
- DMARDs. Arthritis Foundation.
- Clinical Practice Guidelines: Rheumatoid Arthritis. American College of Rheumatology. 2021.
- Complementary and Alternative Medicine for Patients with Rheumatoid Arthritis. Johns Hopkins Arthritis Center.
- Rheumatoid Arthritis and Heart Disease. Arthritis Foundation.
- Hagen KB, Byfuglien MG, Falzon L, et al. Dietary Interventions for Rheumatoid Arthritis. Cochrane Database of Systematic Reviews. January 2009.
- Alwarith J, et al. Nutrition Interventions in Rheumatoid Arthritis: The Potential Use of Plant-Based Diets. A Review. Frontiers in Nutrition. September 2019.
- Hunter TM, Boytsov NN, Zhang X, et al. Prevalence of Rheumatoid Arthritis in the United States Adult Population in Healthcare Claims Databases, 2004–2014, Rheumatology International. September 2017.
- Juvenile Idiopathic Arthritis. MedlinePlus.
- Juvenile Arthritis. American College of Rheumatology. March 2019.
- What Is Arthritis? Arthritis Foundation.
- Osteoarthritis (OA). Centers for Disease Control and Prevention. July 27, 2020.
- What People With Rheumatoid Arthritis Need to Know About Osteoporosis. National Institute of Arthritis and Musculoskeletal and Skin Diseases. November 2018.
- Arthritis and Mental Health. Arthritis Foundation.
- Rheumatoid Arthritis and Lung Problems. Arthritis Foundation.
- Rheumatoid Arthritis and Cancer Risk. Arthritis Foundation.
- Rheumatoid Arthritis. Centers for Disease Control and Prevention. July 27, 2020.
- Dedmon LE. The Genetics of Rheumatoid Arthritis. Rheumatology. October 2020.
- Nguyen Y, Salliot C, Mariette X, et al. Association Between Passive Smoking in Childhood and Adulthood, and Rheumatoid Arthritis: Results From the French E3N-EPIC Cohort Study. Annals of the Rheumatic Diseases. May 19, 2021.
- Abuhelwa et al. Association Between Obesity and Remission in Rheumatoid Arthritis Patients Treated With Disease-Modifying Anti-Rheumatic Drugs. Scientific Reports. October 2020.
- Why Your RA Went Into Remission, but Relapsed. Arthritis Foundation.
- Patient Education: Rheumatoid Arthritis Treatment (Beyond the Basics). UpToDate.
- Complementary and Alternative Medicine for Patients With Rheumatoid Arthritis. Johns Hopkins Arthritis Center.
- Rheumatoid Arthritis and Heart Disease. Arthritis Foundation.
- Alwarith et al. Nutrition Interventions in Rheumatoid Arthritis: The Potential Use of Plant-Based Diets. A Review. Frontiers in Nutrition. September 2019.
- Khanna S, Jaiswal KS, Gupta B. Managing Rheumatoid Arthritis With Dietary Interventions. Frontiers in Nutrition. November 2017.
- Myasoedova, et al. Is the Epidemiology of Rheumatoid Arthritis Changing? Results From a Population-Based Incidence Study, 1985–2014. Annals of the Rheumatic Diseases. March 2020.
- Juvenile Idiopathic Arthritis. MedlinePlus. October 13, 2020.