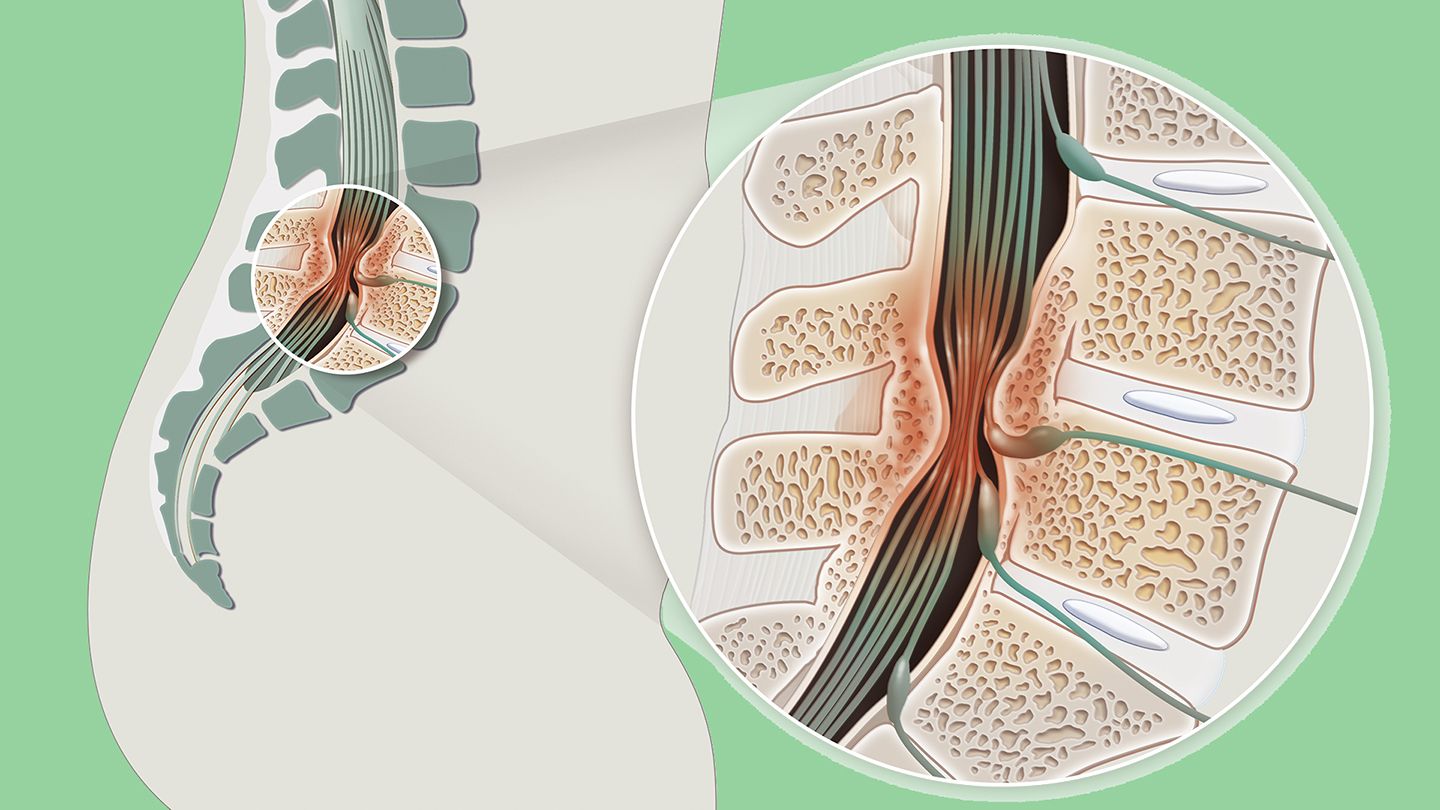
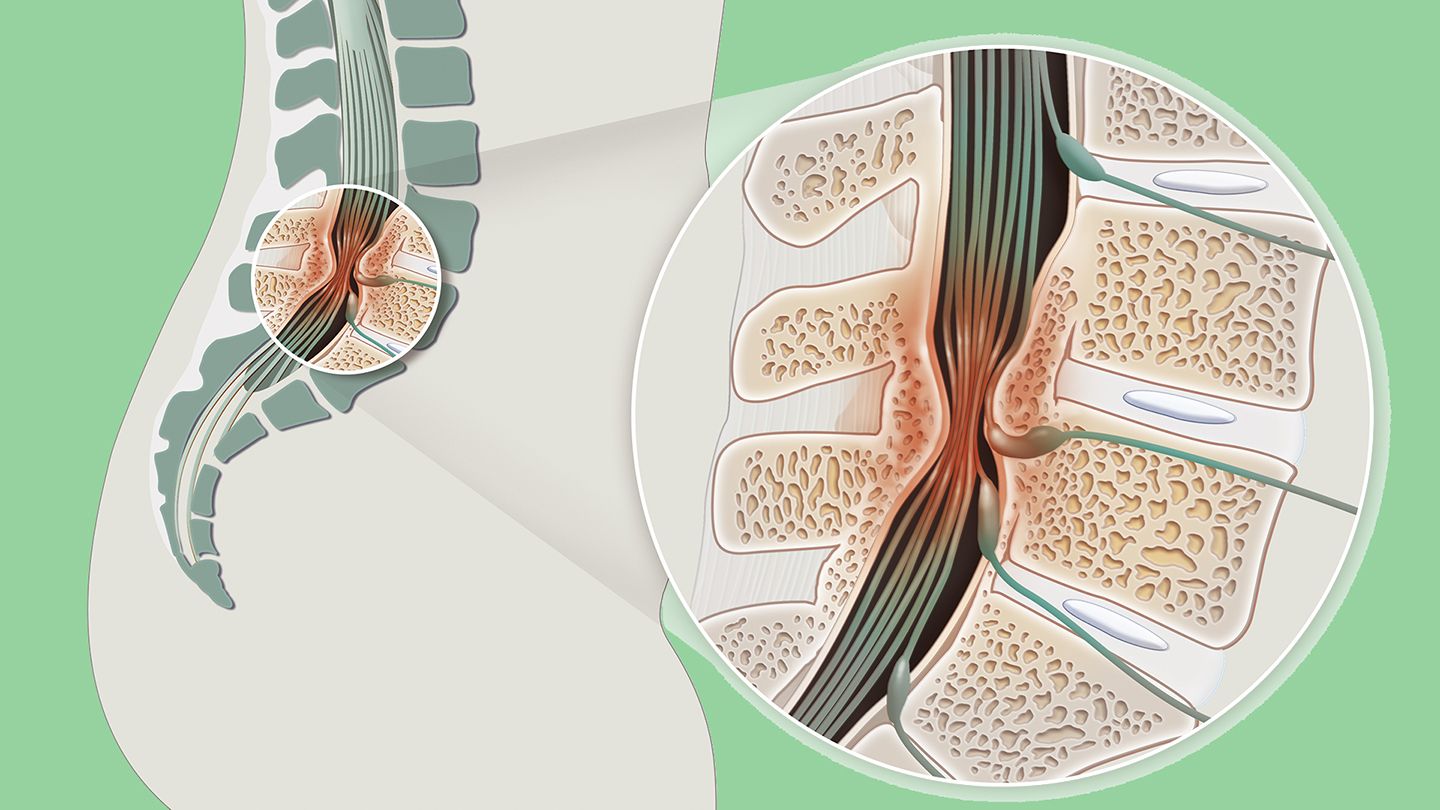
Spinal stenosis — also called vertebral stenosis — is a condition in which spaces in your spine become too narrow (the term “stenosis” refers to narrowing of any passage in the body). As a result, bones or other parts of the spine start pressing on your spinal cord and other nerves.
Although some people don’t experience symptoms, those who do may have pain, numbness, muscle weakness, and tingling in the neck and/or back.
Most people who get spinal stenosis are over age 50. Younger people may develop it if they have certain diseases, get injured, or are born with a narrower-than-usual spine. (1)
Causes and Risk Factors of Spinal Stenosis
Age-related changes to the spine are the main cause of spinal stenosis. Aging bones and ligaments of your spine may gradually get thicker and stiffer, leaving less space between them. Bone spurs that press on the spine and nerves may also develop.
Here are some other risk factors for developing spinal stenosis:
- Osteoarthritis, which involves loss of cartilage in the joints, can trigger excessive bone growth, called bone spurs, that shrinks spinal spaces.
- Rheumatoid arthritis, which causes inflammation and enlargement of soft joint tissues, may also leave less room for the spine and nerves.
- Paget’s disease, which causes excessive bone growth, can affect the spine and result in stenosis.
- Injuries such as herniated disks can also lead to spinal stenosis. And car accidents or other traumatic injuries may leave vertebrae misaligned, leaving less space for nerves.
- Spinal tumors or abnormal growths may press on the spinal cord or nerves, leading to symptoms of stenosis. But this is uncommon. (1)
How Is Spinal Stenosis Diagnosed?
To determine if you have spinal stenosis, your doctor will ask about your symptoms and do a complete physical exam in which they look for signs of spinal stenosis such as numbness and weakness.
It may also be necessary for your doctor to order one of the following tests to confirm the diagnosis:
- X-rays: An X-ray of your back can show bone changes that may be narrowing the spaces in the spinal canal.
- Magnetic resonance imaging (MRI): An MRI creates a cross-sectional image of your spine that can detect where nerves in the spinal cord are under pressure. It can also reveal any damage to disks and ligaments.
- Computed tomography (CT) scan: If you can’t get an MRI, a CT scan can also create images of your spine. It combines X-ray images taken at different angles to produce a cross-sectional picture of your spine. (1)
Duration of Spinal Stenosis
Unfortunately, there isn’t a cure for spinal stenosis. The symptoms tend to start slowly and worsen over time. The good news is there are steps you can take to manage spinal stenosis such as exercising regularly and taking over-the-counter pain relievers. (3)
In rare cases, severe spinal stenosis that’s left untreated can progress and cause permanent weakness, numbness, balance problems, paralysis, and incontinence. (1)
Treatment and Medication Options for Spinal Stenosis
Treatment of spinal stenosis depends on the severity of your symptoms. At-home treatments like stretching and massage therapy can help if your symptoms are mild. If your symptoms are severe, your doctor may recommend medication, physical therapy, or surgery (as a last resort).
Medication Options
- Advil or Motrin (ibuprofen) and other nonsteroidal anti-inflammatory drugs (NSAIDs) can offer relief.
- Antidepressants such as tricyclic antidepressants, which can help ease chronic pain.
- Anti-seizure drugs such as Neurontin (gabapentin) and Lyrica (pregabalin) can decrease pain from damaged nerves.
- Opioids such as oxycodone and hydrocodone may be used for short-term pain relief; however, they are used cautiously since they may become habit-forming.
Steroid injections can also help with the pain (though they don’t cure spinal stenosis). Getting too many steroid injections can weaken bones and connective tissue, so your doctor will likely limit them to a few times a year.
Nonmedicinal Treatments
There are a variety of nonpharmaceutical approaches that, in conjunction with medication, can help ease spinal stenosis symptoms.
- Physical therapy: Your doctor may recommend physical therapy, especially if you’ve become less active due to the pain caused by spinal stenosis. Weak muscles can actually lead to more pain. Working with a physical therapist can help you build strength, become more flexible, and improve your balance.
- Hot or cold packs: Ice packs or hot packs applied to the neck may ease symptoms of stenosis in the cervical region (around the neck). They can also be used on the lower back.
- Weight loss: Losing weight may help ease symptoms of lumbar (lower back) stenosis by reducing the load your spine has to bear. (1)
Alternative and Complementary Treatments
- Chiropractic treatment: Working with a chiropractor may provide some pain relief.
- Acupuncture: Fine needles are used to stimulate specific locations on the body, which may reduce pain.
Prevention of Spinal Stenosis
Unfortunately, there’s no way to prevent spinal stenosis since most people will have some osteoarthritis in their spine by age 50. That said, there are ways to reduce your risk and keep your spine healthy:
- Exercise regularly: Aerobic exercises such as walking, swimming, and cycling can help strengthen your back muscles and help keep your spine flexible.
- Protect your spine: Maintain good posture by sitting in a supportive chair and sleeping on a firm mattress. Avoid lifting heavy objects, or learn how to lift heavy objects safely.
- Keep your weight in check: Being overweight puts excess stress on your back and can cause spinal stenosis. (4)
Complications of Spinal Stenosis
Spinal stenosis can lead to trouble walking due to numbness or weakness, as well as loss of bowel or bladder control. When these complications happen, nonsurgical approaches are usually tried first and can often help. But surgery usually helps ease spinal stenosis symptoms, though symptoms may return even after surgery.
For 'Baby Boomer Back,' Surgery Is Often Good News
Four kinds of surgery are commonly used to treat spinal stenosis:
Laminectomy: In this procedure, a surgeon removes a sizable part of one or more vertebrae to give nerves more room. This may require fusing vertebrae together, or implanting hardware to strengthen the spine.
Laminotomy: In this case, a surgeon removes a smaller portion of a vertebra to relieve some of the pressure.
Laminoplasty: This procedure involves attaching a metal hinge to part of a vertebra. It is only performed on the neck.
Minimally invasive surgery: This technique avoids spinal fusions and results in a quicker recovery time. (1)
Black Americans and Spinal Stenosis
The prevalence of spinal stenosis does not differ by race or ethnicity; however, studies show that African Americans have poorer outcomes after spinal surgery.
According to a study published in May 2020 in the journal Spine, Black patients were 8 percent more likely than white patients to experience spinal fusion surgery complications and 14 percent more likely than white patients to have post-surgery complications. Black patients were also more likely to need longer hospital stays (resulting in higher hospital charges) and were more likely to require 30- and 90-day hospital readmissions.
For the study, researchers looked at discharge records of nearly 268,000 patients almost 78 percent were white and 6.5 percent were Black. The findings are similar to previous studies that have shown how racial disparities impact outcomes after spinal surgery. (7)
Resources We Love
Mayo Clinic
In addition to providing clear, concise information on the symptoms, diagnosis, and treatment of spinal stenosis, the Mayo Clinic also offers advice on how best to prepare for an appointment with your doctor if you’re experiencing the kind of pain and numbness that could be due to this condition.
National Institute of Arthritis and Musculoskeletal and Skin Diseases
This division of the National Institutes of Health offers an up-to-date review on spinal stenosis, as well as details about any clinical trials that may be available.
The American Chronic Pain Association
The ACPA is dedicated to raising awareness about and support and connection for those living with chronic pain conditions, including spinal stenosis. On its website, you can search for a support group near you.
Editorial Sources and Fact-Checking
- Spinal Stenosis. Mayo Clinic. March 8, 2018.
- Spinal Stenosis. National Institute of Arthritis and Musculoskeletal and Skin Diseases. January 2020.
- Spinal Stenosis. American College of Rheumatology. March 2019.
- Lumbar Spinal Stenosis. Johns Hopkins Medicine.
- Lurie, J, Tomkins-Lane C. Management of Lumbar Spinal Stenosis. The BMJ. January 4, 2016.
- Kalichman, L, Cole R, Kim D, et al. Spinal Stenosis Prevalence and Association with Symptoms: the Framingham Study. The Spine Journal. July 9, 2009.
- Aladdin D, Tangel V, Lui B, et al. Black Race as a Social Determinant of Health and Outcomes After Lumbar Spinal Fusion Surgery: A Multistate Analysis, 2007 to 2014. Spine. May 15, 2020.
- Cauda Equina Syndrome. American Association of Neurological Surgeons.